Cost-Containment Strategies for Chronic Weight Management
Exploring the rising costs and demands of weight-loss medication and how to combat those costs, significantly lowering drug costs for payors and increasing access for patients who need them.
Glucagon-like peptide-1 (GLP-1)-based therapies have been gaining steam in the general population and are currently being viewed by patients as an alternative to lifestyle modifications and diet, as opposed to a supplementary intervention. Due to the attention given by social media and news outlets, this therapeutic area has become vulnerable to medication misuse.1 Some of these medications include Ozempic, Mounjaro, and Trulicity, which are all GLP-1 receptor agonists that are FDA-approved for the treatment of diabetes. Drug utilization reports have shown an increase in these anti-diabetes medications that suggest inappropriate use. In contrast, GLP-1-based therapies such as Wegovy, Saxenda, and Zepbound are FDA-approved for weight loss but require specific criteria for use (e.g., for use in adult patients with an initial body mass index (BMI) of 30 kg/m2 or greater).
A recent report showed that GLP-1 therapy utilization had increased 152% as of February 2023 when compared to the previous year, which was only lessened by the shortages developed as a consequence of their over utilization. 2,3 The increase in GLP-1 utilization poses a major budget impact for plan sponsors, as the cost of these drugs can range from $12,000-$18,000 per year.4 Consequently, cost-containment measures are of great value for plan sponsors and payors to ensure appropriate use of weight management programs while minimizing costs for coverage of medications.
Cost-containment methods can be divided as follows:
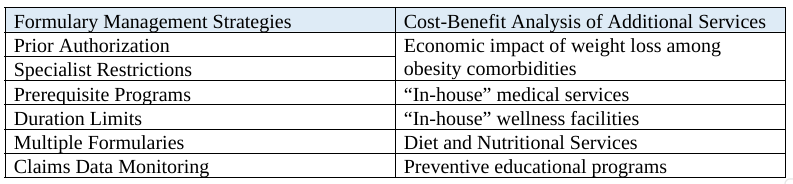
Formulary Management Strategies
Prior Authorization (PA) is a commonly used cost-containment method for plan sponsors that has clinical requirements for the use of certain specialized or high-cost medications. In this approach, specific medical and diagnostic criteria must be met for a plan sponsor to cover a drug. For weight management drugs, ICD-10 diagnosis for obesity is commonly used as a prerequisite for medication coverage. This guarantees that weight-loss drugs are used only by patients that have the proper diagnosis. This prevents potential misuse and overutilization of these medications which, in turn, lowers costs for payors. According to the National Bureau of Economic Research, ensuring proper access to medications with Prior Authorization can reduce utilization by approximately 27%.
5
Prerequisites, Limits & Restrictions
A common benefit adjustment strategy is the implementation of prerequisite programs that precede access to a service or coverage. An example would be the requirement of active member participation in a wellness or nutrition program before getting a prescription for weight-loss medications. Similarly, payors can restrict the coverage of medications to certain specialists to ensure their beneficiaries are receiving the appropriate medications and monitoring. Weight-loss specialists like bariatric doctors or endocrinologists can be established as the sole prescribers for these medications to prevent overuse. This intervention can also help establish the proper duration of therapy as progress and drug discontinuation can be monitored by a specialist. Duration limits for weight-loss medications are also established by taking into account current treatment guidelines for obesity. These guidelines state that if the target weight loss of 5% is not met in a six (6) month period, weight-loss medications should be discontinued or reevaluated. 6
Another approach is to offer multiple plan benefit designs that include or exclude weight-management medications. Drug formularies with an open (more inclusive) plan benefit design may have increased cost sharing for members versus drug formularies with a closed or more restricted benefit. This approach provides members with economic flexibility and the choice in selecting a plan benefit that best adapts to their needs, while also possibly lowering payor costs.
Claims Data Monitoring
Medication prescriptions and claims data should be monitored using retrospective drug utilization reports to ensure the cost-containment strategies are being met and appropriate medication use is being implemented.
Cost-Benefit Analysis Strategies
Cost-benefit analyses are used to evaluate the necessity and effectiveness of additional programs and preventive measures to reduce costs due to weight-loss drugs. Most importantly, in the case of weight management, the internal economic impact should be evaluated to determine if the coverage of weight-loss drugs and programs has produced a noticeable reduction in spending among common obesity comorbidities. Specifically, medical spending in conditions like diabetes, hypertension, dyslipidemia, and osteoarthritis should be evaluated, as weight loss is commonly related to improvement and lower costs in the management of these comorbidities. According to an article from the Journal of Occupational and Environmental Medicine, reductions in 5-20% of BMI (Body Mass Index) can produce significant savings in medical care expenditures ranging from around $500-$6,500 based on the condition studied and the initial BMI of the patient. 7 This report suggests that higher initial BMI, higher percentage of weight loss, and the quantity of initial comorbidities can help predict savings in healthcare costs.
Additional Services
Nutritionist and gym services: These interventions have the potential to prevent obesity on a larger scale. Diet and nutritional services can be offered in the form of practical access to healthy meals and a nutritionist. Furthermore, payors may perform cost-benefit and effectiveness analyses after the implementation of these strategies to demonstrate the economic benefit of these programs.
“In-house” medical services and wellness facilities: The possible financial impact of offering these should be evaluated against the needs of the beneficiaries. The addition of preventive educational programs can aid in highlighting the benefits of lifestyle modifications and boost member motivation. However, cost-benefit analyses should also be completed for these additional strategies since data has not been able to definitively show a relationship between these benefits and the overall cost burden of obesity. 8
In Summary
As weight-loss medications gain popularity with beneficiaries due to their promotion on popular social media platforms, supporting proper medication use accompanied by lifestyle modifications is a priority in the healthcare system. Potential misuse of these medications can cause or worsen drug shortages, which, in turn, limits access for patients. Moreover, improper use and overutilization of these medications can make it impossible for payors to cover weight loss drugs as part of their formulary, which can lead to higher monthly premiums for overall patient health care. The cost-containment strategies expressed above can have a significant impact in lowering drug costs for payors and help promote access to these medications for patients that benefit from their use.
References:
- Chiappini, S., Vickers‐Smith, R., Harris, D. R., Pelletier, G., Corkery, J., Guirguis, A.,
Martinotti, G., Sensi, S. L., & Schifano, F. (2023). Is there a risk for semaglutide misuse? Focus on the Food and Drug Administration’s FDA Adverse Events Reporting System (FAERS) Pharmacovigilance dataset. Pharmaceuticals, 16(7), 994. https://doi.org/10.3390/ph16070994
2. Wojtara, M. S., Syeda, Y., Mozgała, N., & Mazumder, A. (2023). Examining Off-Label Prescribing of Ozempic for
Weight-Loss. Qeios. https://doi.org/10.32388/t6y97s
3. FDA drug shortages. (n.d.). FDA.
https://www.accessdata.fda.gov/scripts/drugshortages/default.cfm
4. Green, L., & Taddei-Allen, P. (2023). Shifting paradigms: Reframing coverage of
Antiobesity medications for plan sponsors. Journal of Managed Care & Specialty Pharmacy, 29(5), 564–568. https://doi.org/10.18553/jmcp.2023.29.5.564
5. Brot-Goldberg, Z., Burn, S., Layton, T. J., & Vabson, B. (2023). Rationing medicine
Through bureaucracy: Authorization restrictions in Medicare. https://doi.org/10.3386/w30878
6. Jensen, M. D., Ryan, D. H., Apovian, C. M., Ard, J. D., Comuzzie, A. G., Donato, K. A.,
Hu, F. B., Hubbard, V. S., Jakicic, J. M., Kushner, R. F., Loria, C. M., Millen, B. E., Nonas, C., Pi‐Sunyer, F. X., Stevens, J., Stevens, V. J., Wadden, T. A., Wolfe, B. M., & Yanovski, S. Z. (2014). 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults. Journal of the American College of Cardiology, 63(25), 2985–3023. https://doi.org/10.1016/j.jacc.2013.11.004
7. Thorpe, K. E., Toles, A., Shah, B. R., Schneider, J., & Bravata, D. M. (2021). Weight
Loss-Associated decreases in medical care expenditures for commercially insured patients with chronic conditions. Journal of Occupational and Environmental Medicine, 63(10), 847–851. https://doi.org/10.1097/jom.0000000000002296
8. Sherman, B., & Addy, C. (2016). Improving engagement in employer-sponsored weight
management programs. PubMed, 22(1), 37–40. https://pubmed.ncbi.nlm.nih.gov/26799123